High Risk Preg. Clinic
Why: High Risk Pregnancy Clinic?
Pregnancy and child bearing are attended by certain risks to the mother as well as the foetus. The aim is to improve our management of the high risk situations and optimize the outcome of pregnancy. With rapid advances in medicine and ready access to information, it is critical for health-care providers to give up-to-date guidance for the workup and management of high-risk pregnancies. Patients today are medically conscious and expect an optimal outcome for their pregnancy.
Classifying pregnancies as “Normal” or “High-Risk” is an effective way to provide additional attention to patients with the greatest need. Some patients have factors at the beginning of pregnancy, such as diabetes or history of a premature delivery that place them in a high-risk category. Others start with normal pregnancies but subsequently develop risk factors, such as ruptured membranes or pregnancies-induced hypertension, which may develop suddenly; therefore, it is critical to be able to identify complications quickly and have a protocol for management. If at 1st visit, your doctor detects that there are some risk factors which are likely to harm you or the baby, you will be advised necessary treatment or hospitalization. It is in your interest to listen to the doctor, follow his/her advice and not ignore it.
Timing of high risk pregnancy All workings days (11 AM-2 PM)
Risk Factors in Pregnancy Mothers with following these factors need more attention in pregnancy and delivery. Do not forget complication can arise in any pregnancy.
| Age |
: |
Less than 18 years; over 35 years |
| Height |
: |
Below 145 cm |
| Weight |
: |
Below 40 kg |
| Parity |
: |
Primi or grandmulti (4 or more previous children) |
| Birth Interval |
: |
Less than 2 years |
| Previous History |
: |
Previous abortions/ premature or still born babies.
Previous difficult delivery of caesarian section, haemorrhage after delivery. |
During Pregnancy
| Pallor or anaemia (Haemoglobin below 10 gm) |
: |
Pallor or anaemia (Haemoglobin below 10 gm) |
| Poor weight gain |
: |
Jaundice |
| Swelling of legs, hands and face |
: |
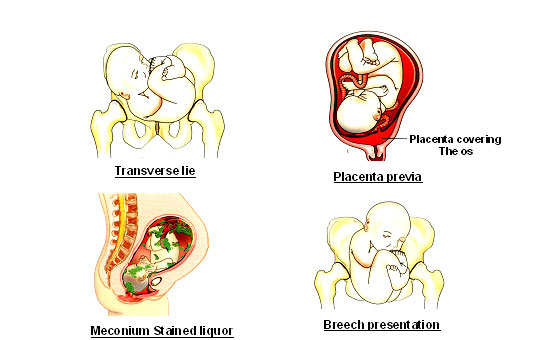
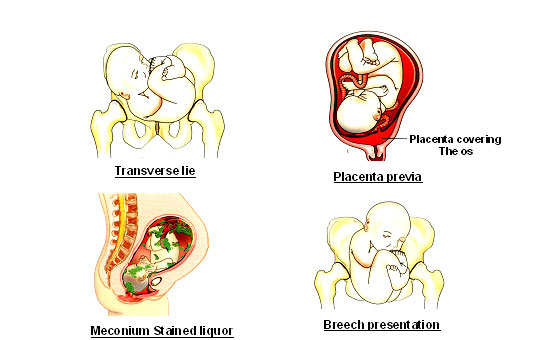
Twins, breech, transverse lie |
| High blood pressure pregnancy |
: |
Prolonged |
| Risk of motherhoodDeveloped world - 1:2800India - 1:175 |
: |
1 in 5 maternaldeaths occur in India only (1.25 lac approximately)75% : Hammorhage; Abortion; Eclampsia; Sepsis; Obs. Labour20% : Anaemia5% Miscellaneous |
| The womb is no longer considered an isolated dark chamber. The foetus is accessible today with increasing clarity with tools such as ultrasonography, magnetic resonance imaging, chorion villus sampling, amniotic fluid studies; Doppler blood flow studies, etc. The concept of the foetus as the The unborn patient has elevated the importance of prenatal diagnosis and treatment. Electronic foetal monitoring of foetal heart is a major breakthrough and very patient friendly procedure. |
Lab Work
Blood tests: Haemoglobin; Haematocrit; and P.B. Smear; VDRL (both partners); Blood group and Rhesus factors (both partners); HbsAg; HIV; GTT (16-20 week); SGOT; SGPT and Serum Creatinine. TSH; TPO; T4; Thalasemia screening.Urine R/E & C/S; Pap Smear; Wet smearUltrasound is safe, non invasive, accurate, fast and cost effective diagnostic test.
A high risk pregnant woman usually undergoes 4 scan.
- Dating cum Viability Scan (6-8 weeks)
- First trimester – Fetal morphology scan 11-14 weeks
- Anomaly scan (18-20 weeks)
- Fetal well being scan (34-35 weeks)